Background
Patellar dislocation occurs when the patella (kneecap) slips out of its groove on the end of the femur (thigh bone). A subluxation is a partial dislocation in which the patella slips but immediately goes back into place. In a full patella dislocation the patella goes back into place as a distinct movement, usually when the knee is straightened. This may occur seconds to hours after the dislocation. When a patella dislocates the chance of another dislocation is immediately quite high, something in the order of 45%. The absolute risk for an individual is difficult to calculate, but it is greater if there are associated predisposing factors. Predisposing factors include: the alignment of the leg, the shape of the groove on the femur for the patella, how high the patella sits in relation to the rest of the knee joint, and the alignment of the foot and ankle. When the patella dislocates on more than one occasion the term recurrent patellar dislocation is used. After two dislocations, the risk of further episodes of dislocation increases in the order of 70 to 80% however it does depend on the time interval between dislocations
Non-Surgical Treatment
If your patella has dislocated only once or maybe twice and you do not have predisposing factors nonsurgical treatment may be recommended. The emphasis of nonsurgical treatment is to build up the quadriceps muscle on the front of the thigh and in particular the vastus medialis (VMO) muscle which is the part of the quadriceps muscle just above the inside of the knee. It is important to do work on strengthening your quads and we will send you to a physiotherapist
Different Surgical Options
If it has been decided that surgery is the appropriate way to manage your condition there are different options that can be used. The particular operation that is selected for you will depend on the alignment of your knee and patella as well as your age. Special X-rays and an MRI scan are used to measure the alignment more accurately and provide further information about the state of the surfaces of your patella Whatever realignment procedure is suggested, it will have an arthroscopy as part of it. The role of the arthroscopy is to clean up any damage on the bone surfaces and to remove any loose fragments .
Medial Patellofemoral Ligament Reconstruction
When the patella dislocates for the first time the structures on the inside of the patella the medial retinaculum tears. A thickening of the retinaculum is called the medial patellofemoral ligament (MPFL). The relocation of the patella causes bone bruises (contusions) on the inside of the patella and outside of the femur
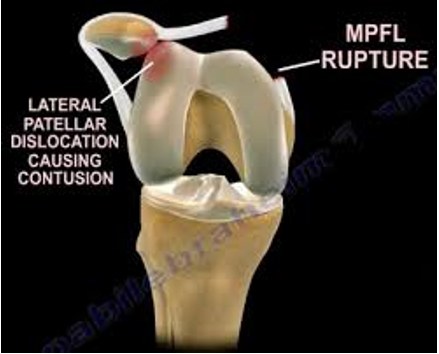
The ligament tear seen on the left image below can be reconstructed by using a hamstring tendon attached to the patella then passed through drill holes made in the femur seen on the right image below. The torn medial retinaculum is also repaired. This involves making three short incisions over the middle and inside part of the knee. The tendon is fixed to the patella with suture anchors and to tunnel with a screw
MPFL reconstruction

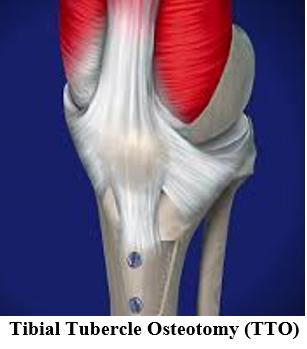
Tibial Tubercle Osteotomy
If the patella is sitting too high, so it’s mostly out of the femoral trochlea groove this increases the risk of ongoing dislocations. It can be moved downwards and into its groove on the femur by moving part of the tibia called the tibial tuberosity. This is the bony lump on the front of the upper end of the shin. The patella is attached to it by the patella tendon. By moving the tuberosity downwards the patella is also moved downwards. Screws are use to hold the tuberosity in its new position. The tibial tuberosity may need to be moved medially, towards inside of the shin in order to improve the tracking of the patella in its groove on the femur. This medial shift may also be combined with a downwards, or distal, shift. Again, the tuberosity is held in place with screws until it heals

Recovery
If you have an MPFL reconstruction you may be able to go home the same day. If you have a TTO or combined procedure you will be in hospital 1-2 nights When you go home you can put weight through your leg and using crutches with pain as your indicator on how much load you put through it. You can discard the crutches once you are safe without them, The focus of the early rehabilitation is to reduce the swelling, restore the function of your quadriceps muscle, and to get the knee bending and straightening normally. If the tibial tuberosity has been moved then it is important to make sure the bone is healed before more aggressive rehabilitation is commenced. Once the swelling has reduced and bone healing has taken place, progression is essentially on ana s tolerated basis. It usually takes up to 3 months before one can recommence running.. Depending on the procedure that has been performed it will take 4 to 6 months to be able to resume sport on a competitive basis.
Complications
- INFECTION: Antibiotics are given at the time of surgery to reduce the risk of infection. Despite this, infection of the wound can occur. This is usually easily treated with antibiotics. However, sometimes the infection gets into the joint which is a serious complication and requires additional surgery.
- THROMBOSIS: A thrombosis is a blood clot that may form in the veins in the legs. This can cause persistent swelling of the foot and ankle and can also be dislodged and be carried to the lungs, resulting in chest pain and breathing difficulties. Once again, the risk is low and blood thinners at the time of surgery as well as following the operation to further reduce the risk. If you develop these you must contact me immediately
- DELAYED BONE HEALING: If a shift of the tibial tuberosity there is a risk that the bone will be slow to heal or may not heal at all. In either case additional surgery may rarely be required to encourage bone healing. The end result is usually satisfactory.
- ONGOING KNEE PAIN: If the medial patellofemoral ligament has been reconstructed there maybe some pain on the inside of the knee with deep flexion where the hamstring graft is. It is usually a matter of working through this. It is not usually a long-term problem. If the hamstring tendon has been harvested to reconstruct the ligament there may be some pain at the back of the knee or thigh s 2 to 6 weeks after surgery. This may be associated with some bruising but this does settle and is not usually a cause any long-term problem. It is important to restore quadriceps function as early as possible. A delayed recovery of quadriceps function may be associated with some shrinking of the patellar tendon. This may pull the patella lower than ideal and may be associated with some pain in front of the knee. The cuts used for surgery may result in some numbness or altered sensation on the front of the knee and shin. This may improve with time. It is common for there to have been some damage to the surface of the patella or femur prior to surgery. This is essentially early osteoarthritis and so there may be some ongoing discomfort at the front of the knee. Avoid patellofemoral activities such as squatting, lunging and knee extension exercises at the gym.
- FURTHER PATELLAR DISLOCATION: Whatever surgery has been performed, there is always a risk of further episodes of patellar dislocation. The risk of a further dislocation is less than 5% as long as you have strengthened your quadriceps.
-
 Source: Understand.com
Source: Understand.com
